
Snapshot
131,953 medical practitioners
- Up 2.2% from 2020/21
- 15.5% of all registered health practitioners
0.5% identified as Aboriginal and/or Torres Strait Islander
45.1% female; 54.9% male
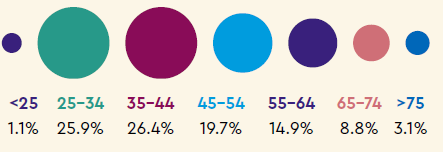
Age
Specialties
| 198 |
addiction medicine |
| 5,793 |
anaesthesia |
| 633 |
dermatology |
| 3,098 |
emergency medicine |
| 34,654 |
general practice |
| 1,126 |
intensive care medicine |
| 355 |
medical administration |
| 2,265 |
obstetrics and gynaecology |
| 308 |
occupational and environmental medicine |
| 1,087 |
ophthalmology |
| 3,621 |
paediatrics and child health |
| 383 |
pain medicine |
| 439 |
palliative medicine |
| 2,375 |
pathology |
| 12,672 |
physician |
| 4,409 |
psychiatry |
| 452 |
public health medicine |
| 453 |
radiation oncology |
| 2,954 |
radiology |
| 591 |
rehabilitation medicine |
| 137 |
sexual health medicine |
| 158 |
sport and exercise medicine |
| 6,441 |
surgery |
| 84,602 |
medical practitioners with specialties |
Regulating
Notifications
6,176 notifications lodged with Ahpra about
4,652 medical practitioners
- 10,873 notifications about 8,146 medical practitioners made Australia-wide, including HPCA and OHO data
- 6.2% of the profession
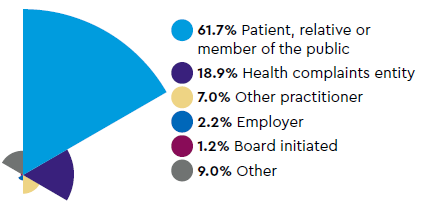
Sources of notifications
Most common types of complaint

344 immediate actions taken
339 mandatory notifications received
- 127 about professional standards
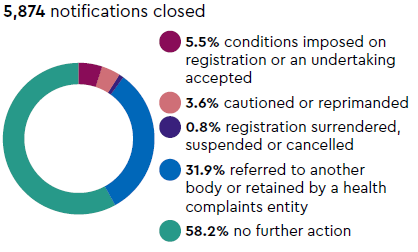
Notifications closed
Monitoring
1,000 practitioners monitored for health, performance and/or conduct during the year
1,303 cases being monitored at 30 June:
- 146 for conduct
- 187 for health
- 278 for performance
- 135 for prohibited practitioner/student
- 557 for suitability/eligibility for registration
Criminal offence complaints
130 criminal offence complaints made
- 88 about title protection
- 2 about practice protection
- 38 about advertising breaches
- 2 other offences
119 closed
Referred to an adjudication body
92 matters decided by a tribunal
1 matter decided by a panel
Appeals
From the Chair
The 2021/22 year was challenging for many of us.
The impact of COVID-19 has been felt deeply, both
professionally and personally. Many of you will be
feeling fatigued and maybe even disillusioned.
The Medical Board of Australia thanks you for your
extraordinary work serving our communities under
challenging circumstances.
Issues this year
COVID-19 continued to feature in our work with
a range of policy decisions to support a surge
workforce and to increase flexibility. The Board is
delighted with the ongoing success of the Medical
Training Survey (MTS) and is grateful for the support
of doctors in training and other stakeholders. We
are disturbed by MTS results across successive
years highlighting unacceptable rates of bullying,
harassment, discrimination and racism. Our Culture
of Medicine Symposium aimed to build a common
understanding of current problems and a shared
commitment to a different future.
We continued our work to strengthen continuing
professional development and improve complaints
handling, and with Ahpra have commissioned an
independent review into cosmetic surgery.
Regulatory responses to COVID-19
The Board made a number of decisions to support
a surge workforce, reduce red tape and support
medical practitioners by:
- establishing an additional pandemic sub-register,
adding to the pool of doctors potentially able to
support the COVID-19 response
- introducing flexibility for 2022 interns whose
internship has been disrupted directly as a result
of COVID-19
- publishing guidance and alerting practitioners
about the Therapeutic Goods Administration’s
restrictions on prescribing ivermectin for
COVID-19
- in partnership with Ahpra, other National Boards,
the Health Care Complaints Commission,
the Office of the Health Ombudsman and the
Therapeutic Goods Administration, publishing a
statement for patients and health consumers to
support informed decision-making, particularly
about sorting fact from fiction
- with Ahpra and the other National Boards,
publishing a statement Facilitating access to
care in a COVID-19 environment: guidance for
health practitioners
- agreeing to temporarily accept additional English
language tests.
Cosmetic surgery independent review
The Medical Board and Ahpra commissioned an
independent review of patient safety issues in the
cosmetic sector, including how to strengthen riskbased
regulation of practitioners in an increasingly
entrepreneurial part of the profession.
Mr Andrew Brown, previously the Queensland Health
Ombudsman, led the review, which included public
consultation.
Professional Performance Framework
The Board’s Professional Performance Framework
continues to guide the work of the Board. It aims to
support registered medical practitioners in Australia
to practise competently and ethically throughout
their careers. It has five pillars:
- Strengthened CPD requirements
- Active assurance of safe practice
- Strengthened assessment and management
of practitioners with multiple substantiated
complaints
- Guidance to support practitioners
- Collaborations to foster a culture of medicine
that is focused on patient safety, is based on
respect and encourages doctors to take care of
their own health and wellbeing
Most of the work described below relates to at least
one pillar.
Medical Training Survey
The Medical Training Survey (MTS) is becoming a
feature of the landscape for doctors in training. This
year, 55% of doctors in training (more than 21,000)
did the survey. Results show that the quality of
training remains high, with improvements reported
in all aspects of the quality of supervision. Of the
surveyed trainees, 80% would recommend their
current training position to other trainees.
Once again, we are deeply concerned about trainee
feedback about the culture of medicine: 35% of
doctors in training reported they had experienced
or witnessed bullying, harassment or discrimination
(including racism). It is even worse for Aboriginal and
Torres Strait Islander doctors in training, with 52%
reporting that they had experienced or witnessed
these unacceptable behaviours.
Results are at www.medicaltrainingsurvey.gov.au. The
MTS is one of the important ways the Board fosters
collaborations to improve the culture of medicine.
Symposium on the culture of medicine
Consistently disturbing findings from the Medical
Training Survey across three years led the Board to
convene a symposium on the culture of medicine
on 27 May. Strong evidence that poor culture is
associated with poor patient outcomes places the
culture of medicine firmly in scope for the Board.
The symposium shared evidence of poor culture
but focused primarily on fostering a commitment to
positive change.
Conference participants identified improved
awareness and understanding of cultural safety,
meaningful action on racism and collaborations to
help effect change as a focus for future effort. We
shared ideas about what we might do together to reshape
the complex system that creates the culture of
medicine in this country.
CPD registration standard
Health Ministers approved the revised CPD
(continuing professional development) registration
standard, which is evidence-based. The revised
standard aims to support medical practitioners to do
high-value CPD that they can incorporate into their
day-to-day practice and create a real and positive
impact. An implementation group was established.
Specialist colleges will transition to become CPD
homes by the end of 2022. Doctors who do their CPD
through their specialist college will therefore meet
the new CPD standard from 1 January 2023. Others
have until 2024 to meet the revised standard.
Health checks for late career
practitioners
The Board’s plan for regular health checks for
practitioners aged 70 and over reflects expert advice
that increasing age is a known risk factor for poor
performance. We developed a draft registration
standard for these health checks and are preparing
a Regulation Impact Statement for consultation.
We expect that most late career practitioners will
continue to practise in their usual way after health
checks are introduced.
Guidance to support practitioners
Registration standard for acupuncture
endorsement
Medical practitioners who want to use the protected
title ‘acupuncturist’ must have their registration
endorsed for acupuncture by the Medical Board
of Australia or also be registered with the Chinese
Medicine Board of Australia. The Medical Board’s
revised registration standard for Endorsement of
registration for acupuncture for registered medical
practitioners defines the requirements, was approved
by Ministers and took effect on 1 July 2022.
International medical graduates
in hospitals
The Board published additional guidance for
hospitals who employ international medical
graduates (IMGs). The guidance supplements
the Board’s Guidelines: supervised practice for
international medical graduates, which are based on
the general practice environment. The information
provides a framework for hospitals to propose
alternative supervision arrangements.
Guidance for IMGs with limited
registration for research
The Board published information for IMGs applying
for limited registration for research positions. It
provides guidance about the evidence an applicant
must provide to show they meet the registration
requirements.
The Board released the cross-profession
Supervised practice framework.
Supervised practice framework
The framework applies to medical practitioners when
supervision is used for the purposes of eligibility or
suitability for registration. For example, when doctors
are returning to practice after a prolonged absence,
changing their scope of practice, or when they are
not able to meet a requirement of a registration
standard. It will also apply when a doctor is required
to complete a period of supervised practice after a
complaint.
The supervised practice framework does not apply
to IMGs with limited or provisional registration, to
interns with provisional registration or to vocational
(specialist) trainees. Supervision requirements for
these medical practitioners have not changed.
Telehealth
The Board reviewed and revised its Guidelines on
technology-based consultations. It will consult on
these in 2022/23.
Stakeholder engagement
Newsletters and media
The Board published 10 regular editions of the
Medical Board Update and two editions of its
medical student newsletter.
The Board responds to many media requests for
comment on a range of issues. We also receive
requests for comment about individual practitioners,
but provide limited information, as permitted by law.
Meetings with stakeholders
The Board has an active program of stakeholder
engagement that includes regular meetings with the:
- Australian Medical Association (AMA)
- Australian Medical Council (AMC)
- Medical Council of New South Wales
- Medical Council of New Zealand
- specialist colleges through the Council of
Presidents of Medical Colleges
- professional indemnity providers
- Drs4Drs – the Board provides about $2m funding
annually for state-based health services for all
medical practitioners and students.
Internal engagement
The Board has a program of internal stakeholder
engagement to promote consistency of decisionmaking
and respond to feedback from our decisionmakers,
including:
- regular meetings with the Chairs of state and
territory boards
- a registration workshop
- the MBA annual conference – an online
conference for all members of the Board and
Ahpra staff.
Stakeholder engagement is a cornerstone of our
regulatory approach and features across all pillars of
the Professional Performance Framework.
Accreditation
The Board considered each of the AMC’s
accreditation reports and decided whether to
approve the relevant accredited program of study
for registration.
New fields and specialties
The Board progressed rural generalist medicine as a
new field of specialty practice within general practice
to the second stage of assessment, which includes a
detailed assessment, including public consultation.
The Board sought advice from the AMC about
an application for recognition of clinical forensic
medicine as a new specialty.
Managing complaints
The Board and Ahpra appreciate the enormous
stress that many medical practitioners experience
when a notification (complaint) is made about them.
Our own research tells us that the longer it takes to
resolve a notification, the more distressing it is for
everyone involved.
The Board continues to make changes to improve the
management of complaints, including:
- changing the scope of the Sexual Boundaries
Notifications Committee to include matters
involving family violence
- establishing a national committee to deal with all
COVID-19-related notifications
- continuing its risk-based approach, by dealing
with low-risk matters quickly and focusing
resources on high-risk matters; the Notifications
Assessment Committee meets six times each
week – a measure of the complaints-handling
workload.
Dr Anne Tonkin
